A Physician's Guide to Radon
This booklet on radon has been developed for physicians by the U.S. Environmental Protection Agency in consultation with the American Medical Association (AMA). Its purpose is to enlist physicians in the national effort to inform the American public about the serious health risk posed by indoor radon gas.
- Introduction
Lung cancer's very high associated mortality rate is even more tragic because a significant portion of lung cancer is preventable. While smoking remains the number one cause of lung cancer, radon presents a significant second risk factor. That is why, in addition to encouraging patients to stop smoking, it is important for physicians to inquire about and encourage patients to test for radon levels in their homes. One way to do this is for physicians to join those health care professionals and organizations who have begun to include questions about the radon level in patients' homes on standardized patient history forms.
Because the public views physicians as advisors on health and prevention of disease, physicians are in a unique position to play a vital role in informing the public about the common and serious risk of radon, and in educating their patients in testing procedures and remediation methods for correcting elevated indoor radon levels, thereby helping to reduce the number of lung cancer deaths.
- You can also contact your state radon office to assist you in educating your patients about radon.
- Executive Summary
Radon Causes Thousands Of Preventable Lung Cancer Deaths Each Year
Each year in the United States exposure to indoor radon gas causes thousands of preventable lung cancer deaths. In fact, the Surgeon General has warned that radon is the second leading cause of lung cancer in the United States. Extensive epidemiological evidence from studies of underground miners, complemented by animal data, indicates that radon causes lung cancer in both smokers and nonsmokers, although malignancy is especially likely to occur in cigarette smokers. Exposure to both smoking and radon greatly enhances the risk of lung cancer. The carcinogenicity of radon is supported by a consensus of opinion among national and international health organizations. By informing patients about the health risk posed by radon exposure and providing practical advice about radon testing and mitigation, physicians can have a tremendous positive impact on the national effort to prevent radon-induced lung cancer.
Radon is estimated to cause about 14,000 deaths per year, however, this number could range from 7,000 to 30,000 deaths per year. The numbers of deaths from other causes are taken from the 1990 National Safety Council reports.
According to the Office of the Surgeon General: Indoor radon gas is a serious health problem in our nation that can be addressed by individual action. Unless people become aware of the danger radon poses, they will not act. Millions of homes are estimated to have elevated radon levels. Fortunately, the solution to this problem is straight-forward. Like the hazards from smoking, the health risks of radon can be reduced.
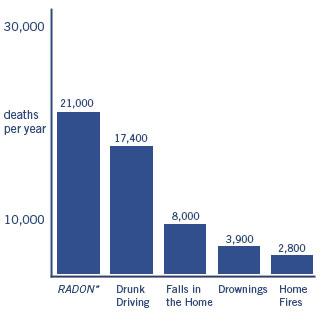 EPA estimates that radon causes thousands of cancer deaths in the U.S. each year.
EPA estimates that radon causes thousands of cancer deaths in the U.S. each year.* Radon is estimated to cause about 21,000 lung cancer deaths per year, according to EPA's 2003 Assessment of Risks from Radon in Homes (EPA 402-R-03-003). The numbers of deaths from other causes are taken from the Centers for Disease Control and Prevention's 2005-2006 National Center for Injury Prevention and Control Report and 2006 National Safety Council Reports.
Radon Is Easy To Detect And Reduce In A Home
The danger posed by radon can be detected rather easily through inexpensive do-it yourself testing, or through a trained radon contractor. Radon test kits can be purchased by mail order or in hardware stores and other retail outlets. Because of the serious health risk posed by radon, the U.S. Environmental Protection Agency (EPA) recommends that all homes be tested for radon below the third floor.
If an elevated radon level is discovered in a home, it can be corrected. It is recommended that a confirmed radon level of four picocuries per liter (pCi/L) of air or higher be reduced to decrease the risk of developing lung cancer. The cost of radon mitigation in a typical home ranges from about $500 to about $2,500. Your state radon information office (see page toward end of this brochure) can provide general advice about radon testing and mitigation, as well as specific information about qualified radon contractors in your state.
- What is Radon?
Radon-222 is a radioactive gas released during the natural decay of thorium and uranium, which are common, naturally occurring elements found in varying amounts in rock and soil. Odorless, invisible, and without taste, radon cannot be detected with the human senses.
Radon-222 decays into radioactive elements, two of which, polonium-218 and polonium-214, emit alpha particles, which are highly effective in damaging lung tissues. These alpha-emitting radon decay products have been implicated in a causal relationship with lung cancer in humans.
- Characteristics and Sources of Radon
Outdoors, where it is diluted to low concentrations in the air, radon poses significantly less risk than indoors. In the indoor air environment, however, radon can accumulate to significant levels. The magnitude of radon concentration indoors depends primarily on a building's construction and the amount of radon in the underlying soil. The soil composition under and around a house affects radon levels and the ease with which radon migrates toward a house. Normal pressure differences between the house and the soil can create a slight vacuum in the home that can draw radon gas from the soil into the building.
Radon gas can enter a home from the soil through cracks in:
- concrete floors and walls
- floor drains, sump pumps
- construction joints
- and tiny cracks or pores in hollow-block walls
Radon levels are generally highest in basements and ground floor rooms that are in contact with the soil. Factors such as the design, construction and ventilation of the home affect the pathways and sources that can draw radon indoors. Another source of radon indoors may be air released by well water during showering and other household activities. Compared to radon entering the home through soil, radon entering the home through water will in most cases be a small source of risk.
- Cracks in concrete slabs
- Spaces behind brick veneer walls that rest on uncapped hollow-brick foundation
- Pores and cracks in concrete blocks
- Floor-wall joints
- Exposed soil, as in a sump
- Weeping (drain) tile, if drained to open sump
- Mortar joints
- Loose fitting pipe penetrations
- Open tops of block walls
- Building materials such as some rocks
- Water (from some wells)
- The Health Risk
How Does Radon Induce Cancer?
If inhaled, radon decay products (polonium-218 and polonium-214, solid form), unattached or attached to the surface of aerosols, dusts and smoke particles, become deeply lodged or trapped in the lungs, where they can radiate and penetrate the cells of mucous membranes, bronchi and other pulmonary tissues. The ionizing radiation energy affecting the bronchial epithelial cells is believed to initiate the process of carcinogenesis. Although radon-related lung cancers are mainly seen in the upper airways, radon increases the incidence of all histological types of lung cancer, including small cell carcinoma, Aden carcinoma and squamous cell carcinoma. Lung cancer due to inhalation of radon decay products constitutes the only known risk associated with radon. In studies done on miners, variables such as age, duration of exposure, time since initiation of exposure and especially the use of tobacco have been found to influence individual risk. In fact, the use of tobacco multiplies the risk of radon-induced lung cancer enormously.
What is the Evidence?
More is known about the health risk of radon exposure to humans than about most other human carcinogens. This knowledge is based on extensive epidemiological studies of thousands of underground miners, carried out over more than fifty (50) years world-wide, including miners in the United States and Canada. In addition to the miner data, experimental exposures of animals confirm that radon and its decay products can cause lung cancer.
The research on lung cancer mortality in miners exposed to radon progeny is substantial and consistent. Studies of thousands of miners, some with follow-up periods of thirty (30) years and more, have been conducted in metal, fluorspar, shale, and uranium mines in the United States, Canada, Australia, China, and Europe. These studies have consistently shown an increase in lung cancer occurrence with exposure to radon decay products, despite differences in study populations and methodologies.
The miner studies produced some interesting findings.
- At equal cumulative exposures, low exposures in the range of EPA's 4 pCi/L action level over longer periods produced greater lung cancer risk than high exposures over short periods.
- Increased lung cancer risk with radon exposure has been observed even after controlling for, or in the absence of, other mine exposures such as asbestos, silica, diesel fumes, arsenic, chromium, nickel and ore dust.
- Increased lung cancer risk has been observed in miners at relatively low cumulative exposures in the range of EPA's 4 pCi/L action level (Sevc Kunz, Tomasik et al, Health Physics 54(1):27-46,1988; Mulles Wheeler et al, Proceedings of International Conference on Occupation Radiation Safety in Mining, Vol. 1, Canadian Nuclear Association; Radford and St. Clair Renard, New England Journal of Medicine 310(23):1485-1494, 1984;Woodward, Roder et al, "Cancer Causes and Control" 2:213-220, 1991).
- Nonsmoking miners exposed to radon have been observed to have an increased risk of lung cancer.
The following table lists seven (7) of the major epidemiological studies of underground miners and their reported relative risk coefficients.
Estimates of Lung Cancer Risk From Epidemiological Studies of Underground Miners Exposed to Radon
Study Population
Average Exposure
(WLM)a.Relative Risk
Coefficient
(%/WLM)b.
ReferencesCzech Uranium Miners 313
2261.92
1.5Thomas et al. 1985
Sevc et al. 1988Ontario Uranium Miners
40-900.5-1.3
1.4c.Muler 1984
NAS 1988New Mexico Uranium Miners 111.4 1.8 Samet et al. 1991 Swedish Iron Miners (Malmberget) 81.4 3.6
1.4c.Radford & St. Clair Renard 1984
NAS 1988Colorado Plateau Uranium Miners 834 .45
.06c.Thomas et al. 1985
NAS 1988Eldorado (Beaverlodge) Uranium Miners 20.2 3.28
2.6Howe et al. 1986
NAS 1988Newfoundland Fluorospar Miners 382.2 0.9 Morrison et al. 1988 a. = Working level month (WLM) is the cumulative exposure equivalent to one (1) working level (WL) for a working month (170 hours). A WL is any combination of short-lived radon daughters in one (1) liter of air that will result in the emission of 1.3 x 105 MeV of potential alpha energy. A home exposure of 4 pCi/L for seventy (70) years would approximately equal a cumulative exposure of 54 WLM
(assuming 75% occupancy).
b. = The relative risk coefficient is the fractional increase above the baseline lung cancer incidence or mortality rate per WLM. For example, the Czech Uranium Miner demonstrated a 1.92% increased lung cancer risk for every WLM of exposure. Exposure to five (5) WLM would therefore increase lung cancer risk by 9.6% over baseline.
c. = Estimate based on reanalysis of the data by the NAS with the cooperation of the principal investigators.
* The excess relative risk coefficient used in EPA's risk assessment (1.3%/WLM) is that derived by the NAS BEIR IV report based on their analysis of studies of underground mines.
A detailed discussion of the strengths and weaknesses of the various miner studies can be found in the EPA's Technical Support document for the 1992 Citizen's Guide to Radon or the BEIR IV Report (National Academy of Sciences (NAS) 1988).Animal experiments conducted in the United States and France also have confirmed the carcinogenicity of radon and have provided insight into the nature of the exposure-response relationship, as well as the modifying effects of the exposure rate. To date these animal studies have produced several relevant findings.
- Health effects observed in animals exposed to radon and radon decay products include lung carcinomas, pulmonary fibrosis, emphysema and a shortening of life-span (U.S. DOE/Office of Energy Research 1988a).
- The incidence of respiratory tract tumors increased with an increase in cumulative exposure and with a decrease in rate of exposure (NAS 1988).
- Increased incidence of respiratory tract tumors was observed in rats at cumulative exposures as low as 20 WLM (NAS 1988).
- Exposure to ore dust or diesel fumes simultaneously with radon did not increase the incidence of lung tumors above that produced by radon progeny exposures alone (DOE/Office of Energy Research 1988a).
- Lifetime lung-tumor risk coefficients that have been observed in animals are similar to the life-time lung-cancer risk coefficients observed in human studies (DOE/Office of Energy Research 1988a).
- In a study of rats exposed to radon progeny and uranium ore dust simultaneously, it was observed that the risk of lung cancer was elevated at exposure levels similar to those found in homes. The risk decreased in proportion to the decrease in radon -progeny exposure (Cross et al, 1991).
In 1988, a panel of world experts convened by the World Health Organization's International Agency for Research on Cancer unanimously agreed that there is sufficient evidence to conclude that radon causes cancer in humans and in laboratory animals (IARC, 1988). Scientific committees assembled by the National Academy of Sciences (NAS, 1988), the International Commission on Radiological Protection (ICRP, 1987), and the National Council on Radiation Protection and Measurement (NCRP, 1984) also have reviewed the available data and agreed that radon exposure causes human lung cancer.
Recognizing that radon is a significant public health risk, scientific and professional organizations such as the American Medical Association, the American Lung Association, and the National Medical Association have developed programs to reduce the health risks of radon. The National Institute for Occupational Safety and Health (NIOSH) reviewed the epidemiological data and recommended that the annual radon progeny exposure limit for the mining industry be lowered (NIOSH 1987).
Is Occupational Exposure to Radon Comparable to Residential Exposure?
Because questions have been raised about the appropriateness of using the epidemiological studies of underground miners as a basis for estimating the risk radon poses to the general population, the EPA commissioned the National Academy of Sciences (NAS) to investigate the difference between underground miners and members of the general public in the doses they receive per unit exposure due to inhaled radon progeny.
The NAS report, published in 1991 (National Academy of Sciences, 1991, Comparative Dosimetry of Radon in Mines and Homes. National Academy Press, Washington, D.C.), concluded that it is reasonable to extrapolate from the miner data to a residential situation, but that the effective doses per unit of exposure for people in their homes is approximately thirty percent (30%) less than for the miners. In its analysis, NAS considered variables such as the amount and type of dust to which the radon decay particles would attach, the breathing rate of working miners compared to that of people at home, and the presence of women and children in the homes.
EPA has adjusted its residential risk estimates accordingly. The result is still considerable -- EPA now estimates that approximately 14,000 lung cancer deaths in the United States per year are due to residential radon exposures, with an uncertainty range of 7,000 to 30,000. As more data are gathered about residential radon exposures, the risk estimates may be adjusted further. Enough data exists now, however, to be able to say with certainty that thousands of preventable lung cancer deaths annually in the United States are attributable to indoor residential exposure to radon.
More information about residential exposure to radon is needed to answer important questions about radon's effect on women and children -- groups not included in the occupational studies of miners. Although children have been reported to be at greater risk than adults of developing certain types of cancer from radiation, currently there is no conclusive evidence that radon exposure places children at any greater risk. Some miner studies and animal studies indicate that for the same total exposure, a lower exposure over a longer time is more hazardous than short, high exposures. These findings increase concerns about residential radon exposures. Epidemiological case control studies are underway in the U.S. and Europe, the pooled results of which should enhance the understanding of the risk of residential exposure to radon.
What About Smoking and Radon Exposure?
Some people ask whether the lung cancer deaths attributed to radon exposure actually may be the result of smoking. A 1989 study by researchers from the National Institute for Occupational Safety and Health, the Centers for Disease Control, the Harvard School of Public Health, and the University of California at Davis demonstrated a greatly incased lung cancer risk in nonsmoking uranium miners exposed to high radon concentrations: compared to typical non-smoking populations, these miners had nine (9) to twelve (12) times the risk of developing lung cancer (Roscoe et al, JAMA 262(5): 629-633, 1989).
Evidence from some of the epidemiological studies of underground miners, primarily U. S. uranium miners, indicate that radon exposure and smoking may have a synergistic relationship. Either smoking or radon exposure can independently increase the risk of lung cancer; however, exposure to both greatly enhances that risk.
Your chances of getting lung cancer from radon depend mostly on:
- How much radon is in your home
- The amount of time you spend in your home
- Whether you are a smoker or have ever smoked
Radon Risk If You Smoke
Radon Level If 1,000 people who smoked were exposed to this level over a lifetime*... The risk of cancer from radon exposure compares to**... WHAT TO DO:
Stop smoking and...20 pCi/L About 260 people could get lung cancer 250 times the risk of drowning Fix your home 10 pCi/L About 150 people could get lung cancer 200 times the risk of dying in a home fire Fix your home 8 pCi/L About 120 people could get lung cancer 30 times the risk of dying in a fall Fix your home 4 pCi/L About 62 people could get lung cancer 5 times the risk of dying in a car crash Fix your home 2 pCi/L About 32 people could get lung cancer 6 times the risk of dying from poison Consider fixing between 2 and 4 pCi/L 1.3 pCi/L About 20 people could get lung cancer (Average indoor radon level) (Reducing radon
levels below 2 pCi/L is difficult.)0.4 pCi/L About 3 people could get lung cancer (Average outdoor radon level) Note: If you are a former smoker, your risk may be lower.
* Lifetime risk of lung cancer deaths from EPA Assessment of Risks from Radon in Homes (EPA 402-R-03-003).
** Comparison data calculated using the Centers for Disease Control and Prevention's 1999-2001 National Center for Injury Prevention and Control Reports.Radon Risk If You've Never Smoked
Radon Level If 1,000 people who never smoked were exposed to this level over a lifetime*... The risk of cancer from radon exposure compares to**... WHAT TO DO: 20 pCi/L About 36 people could get lung cancer 35 times the risk of drowning Fix your home 10 pCi/L About 18 people could get lung cancer 20 times the risk of dying in a home fire Fix your home 8 pCi/L About 15 people could get lung cancer 4 times the risk of dying in a fall Fix your home 4 pCi/L About 7 people could get lung cancer The risk of dying in a car crash Fix your home 2 pCi/L About 4 person could get lung cancer The risk of dying from poison Consider fixing between 2 and 4 pCi/L 1.3 pCi/L About 2 people could get lung cancer (Average indoor radon level) (Reducing radon levels below
2 pCi/L is difficult.)0.4 pCi/L (Average outdoor radon level) Note: If you are a former smoker, your risk may be higher.
* Lifetime risk of lung cancer deaths from EPA Assessment of Risks from Radon in Homes (EPA 402-R-03-003).
** Comparison data calculated using the Centers for Disease Control and Prevention's 1999-2001 National Center for Injury Prevention and Control Reports.Why Should Every Home be Tested?
The EPA and the U. S. Surgeon General recommend testing all homes below the third floor for radon. Data gathered by the EPA national radon survey indicate that elevated radon levels are present in about six million (6,000,000) homes throughout the United States. In every state there are homes with dangerously high radon levels. Because the radon concentration inside a home is due to factors relating to its structure and geographic location, each individual home must be tested to determine its radon level. Two adjacent houses may have radically different radon levels. And any kind of home can have elevated levels, new or old, drafty or well-sealed and basement or non-basement.
How do You Obtain a Reliable Test Result?
Although radon cannot be seen or smelled, with the proper equipment its presence is relatively easy to detect.
The EPA operated a voluntary National Radon Proficiency (RPP) Program that evaluated radon measurement companies and the test services they offer until 1998. You can find out how to find a "qualified" Radon Service Professional in your area.
Radon Testing Methods
The quickest way to test for radon is with a short-term "do-it-yourself" radon test kit, available by mail order and in many retail outlets or by hiring an EPA qualified or state-certified radon tester. Common short-term test devices are charcoal canisters, alpha track detectors, liquid scintillation detectors, electret ion chambers, and continuous monitors. A short-term testing device remains in the home for two (2) to ninety (90) days, depending on the type of device. Because radon levels tend to vary from day-to-day and season-to-season, a long-term test is more likely than a short-term test to measure the home's year-round average radon level. If results are needed quickly, however, a short-term test followed by a second short-term test may be used to determine the severity of the radon problem.
Long-term test devices, comparable in cost to devices for short-term testing, remain in the home for more than three (3) months. A long-term test is more likely to indicate the home's year-round average radon level than a short-term test. Alpha track detectors and electret ion detectors are the most common long-term test devices.
Radon Test Devices
Charcoal canister and liquid scintillation detectors contain small quantities of activated charcoal. Radon and its decay products are absorbed onto the charcoal and are measured by counting with a sodium iodide detector or a liquid scintillation counter.
Alpha track detectors contain a small sheet of plastic that is exposed for a period of one (1) to three (3) months. Alpha particles etch the plastic as they strike it. These marks are then chemically treated and counted in the laboratory to determine the radon concentration.
Electret ion detectors contain an electro statically charged Teflon disk. Ions generated by the decay of radon strike and reduce the surface voltage of the disk. By measuring the voltage reduction, the radon concentration can be calculated.
Continuous monitors are active devices which need power to function. They require operation by trained testers and work by continuously measuring and recording the amount of radon in the home.
How To Test
During a short-term test, doors and windows are closed twelve (12) hours prior to testing and throughout the testing period. (A short-term test lasting two (2) or three (3) days should not be conducted during unusually severe storms or periods of unusually high winds.) The test kit is placed in the lowest lived-in level of the home, at least twenty (20) inches above the floor, in a room that is used regularly, but not in the kitchen or bathroom where high humidity or the operation of an exhaust fan could affect the validity of the test. At the end of the test period, the kit is mailed to a laboratory for analysis; results are mailed back in a few weeks.
In some cases, such as real estate transactions, "qualified" or state-certified contractors conduct the radon test. The EPA's guidance Home Buyer's and Seller's Guide to Radon addresses issues during real estate transactions.
Interpreting Radon Test Results
- If the short-term test result is 4 pCi/L or higher, conduct a follow-up test to confirm the results.
- Follow-up with either a long-term test or a second short-term test.
- For a better understanding of the home's year-round average radon level, take a long-term test.
- If results are needed quickly, take a second short-term test.
- The higher the initial short-term result, the more certain the homeowner can be to conduct a short-term rather than a long-term follow-up test. If the first short-term test result is several times the action level - for example, about 10 pCi/L or higher - a second short-term test should be taken immediately.
- If the long-term follow-up test result is 4 pCi/L or more, fix the home.
- If the homeowner followed up with a second short-term test: the higher the short-term results, the more certain the homeowner can be that the home should be fixed. The homeowner should consider fixing the home if the average of the first and second test is 4 pCi/L or higher.
Basis for the 4 pCi/L Radon "Action Level"
No radon level is considered "safe". The risk of developing lung cancer is directly proportional to the levels and duration of exposure to radon: the higher the radon concentration, the higher the lung cancer risk. The 4 pCi/L "Action Level" is based on current mitigation technology. Today, mitigation technology can almost always reduce high radon concentration levels to below 4 pCi/l and to 2 pCi/L or below 70-80 percent of the time. The average radon level in homes is about 1.25 pCi/L. Although Congress passed legislation in 1988 establishing a national goal that indoor radon levels not exceed ambient outdoor radon levels (0.2-0.7 pCi/L), this goal is not yet technologically achievable.
Radon Reduction Methods
Radon in soil is drawn indoors by the differential between the relatively low air pressure in the house and the higher air pressure in the soil. Therefore, radon reduction strategies fall into two basic categories: those that prevent the entry of radon gas into the home, and those that attempt to remove the radon once it has entered the home. In most situations, the first approach -- preventing radon entry -- is the most effective.
Although sealing cracks and other openings in the foundation is a basic part of most approaches to radon reduction, sealing alone is not recommended; it is best done in conjunction with other mitigation techniques to enhance their effectiveness.
The most popular radon mitigation technology is called "sub-slab depressurization" or "sub-slab suction." The "sub-slab depressurization" technique removes radon-laden air from beneath the foundation and vents it outside the house by installing a fan and inserting a pipe through the foundation into the aggregate below, running it to a point outside the shell of the house. A similar technique, "sub-membrane depressurization," which is effective in buildings with earth-floored crawlspaces or basements, uses a plastic barrier over the soil as a collection cover. Another depressurization technique for preventing radon entry, "blockwall depressurization," uses a fan and duct work to draw suction on the hollow interior cavities of a concrete block wall. By keeping the air pressure within the block wall lower than the air pressure in the basement, the soil gas is removed before it can enter the basement.
Reducing radon levels requires technical knowledge and special skills. The EPA operated a Radon Contractor Proficiency (RCP) Program that evaluated radon reduction contractors until 1998. Selecting a radon contractor is much like choosing a contractor for other home repairs; it makes sense to get references and more than one estimate. The average cost to correct a radon problem in a home is about $1,200, although it can range from about $500 to about $2,500. You can order a free copy of A Consumer's Guide to Radon Reduction. People who choose to fix their homes themselves should refer to the EPA's technical guide, Radon Reduction Techniques for Detached Houses.
After the radon reduction procedure is complete, the home should be retested. Most radon reduction systems include a monitor that will alert the homeowner if the system needs servicing.
- Other Indoor Air Pollutants
Environmental Tobacco Smoke (ETS)
The U. S. Environmental Protection Agency has classified environmental tobacco smoke (ETS) as a Group A (known human) carcinogen. EPA estimates that approximately 3,000 lung cancer deaths in the United States per year among nonsmokers are due to ETS. The U.S. Surgeon General, the National Research Council, and the National Institute for Occupational Safety and Health have all concluded that passive smoking can cause lung cancer in otherwise healthy adults who never smoked.
Children's lungs are even more susceptible to harmful effects from ETS. In infants and young children up to three years, exposure to ETS causes an approximate doubling in the incidence of pneumonia, bronchitis, and bronchiolitis. There is also strong evidence of increased middle ear effusion and reduced lung function and lung growth. Several recent studies link ETS with increased incidence and prevalence of asthma and increased severity of asthmatic symptoms in children of mothers who smoke heavily.
Environmental tobacco smoke is a complex mixture of more than 4,000 chemicals found in both vapor and particle phases, many known toxic and carcinogenic agents. ETS consists of both "sidestream" smoke, the emission from the burning end of the cigarette, and exhaled "mainstream smoke," the smoke inhaled by the active smoker.
Biological Air Pollutants
Dust mites, molds, animal dander, and other biologicals are found in some degree in every home and workplace. High relative humidity is the primary factor encouraging biological agents to grow and be released into the air. Biological agents are known to cause three types of human diseases: infections, where pathogens invade human tissues; hypersensitivity diseases, where specific activation of the immune system causes disease; and toxicoses, where biologically produced chemical toxins cause direct toxic effects.
Volatile Organic Compounds (VOCs)
Volatile Organic Compounds (VOCs) are emitted as vapors or gases at ordinary temperatures from a variety of sources. Many are toxic, including benzene, carbon tetrachloride, and formaldehyde. VOCs can be found in paint, upholstery, spray cans, copy machine toners, clothing, and other sources. Health effects range from irritation of the eyes and respiratory system to kidney or liver damage, cancer, or birth defects.
Other Combustion Products
Aside from ETS, the major combustion pollutants that may be present at harmful levels in the home or workplace stem chiefly from malfunctioning or misusing heating devices.
- carbon monoxide (CO)
- nitrogen dioxide (NO2)
- sulfur dioxide (SO2)
An additional source of exposure may be motor vehicle emissions as a result of a garage or loading dock located near air intake vents. Symptoms may mimic influenza during the heating season and include:
- fatigue
- nausea
- dizziness
- headaches
- cognitive impairment
- tachycardia
For more information on these and other indoor air pollutants, see our:
- Indoor Air Pollution: An Introduction for Health Professionals
- The Inside Story: A Guide to Indoor Air Quality
Preventive Measures That Can Be Taken to Reduce Your Exposure to Indoor Air Pollutants Include the Following:
Environmental Tobacco Smoke (ETS)
- Don't' smoke around others, particularly children.
- Every organization dealing with children should have a smoking policy that effectively protects children from ETS.
- In the work place, prohibit smoking indoors or provide separately ventilated smoking areas.
- If smoking is permitted in restaurants and bars, placement of smoking areas should be designated to minimize nonsmoker exposure.
- Read more at the SmokeFree website
Biological Air Pollutants
- Provide adequate outdoor air ventilation.
- Keep equipment water reservoirs clean.
- Eliminate standing water, wash bedding and soft toys frequently in hot water.
- Vacuum carpets and upholstered furniture regularly.
- Read more about Biologic Pollutants
Volatile Organic Compounds (VOCs)
- Remove the source.
- Avoid use.
- Increase ventilation when using products.
- Read more about Volatile Organic Compounds
Other Combustion Products
- Vent furnaces, water heaters and clothes dryers to the outdoors.
- Periodic professional inspections and maintenance of major appliances.
- Regularly clean fireplace and wood/coal stove flues.
- Read more about Carbon Monoxide
- Most Commonly Asked Questions About Radon
Q. Where does radon come from?
A. Radon is a naturally occurring gas that results from the breakdown of uranium commonly found in soil.
Q. How does radon enter my home?
A. Radon comes up through the soil and rocks surrounding your home and seeps through cracks in concrete walls and floors, floor drains, sump pumps, joints, and hollow-brick walls.
Q. Why haven't I heard of the radon danger until recently?
A. Radon has always existed. However, it was not until the 1980s that dangerous radon levels were found inside homes across the U.S.
Q. What are the health risks?
A. Radon is the second leading cause of lung cancer.
Q. How do I know if I have radon in my home?
A. By testing with an EPA-listed or State-certified easy-to-use, inexpensive test kit as soon as possible, or by hiring an EPA-listed or State-certified contractor to test your home for you.
Q. If I have a radon problem, can it be corrected?
A. Yes. The use of trained personnel is recommended. State radon offices can recommend qualified contractors. In some cases, the problem can be treated by the homeowners if they have experience with other kinds of home repair.
Q. Will my neighbor's radon measurement indicate whether or not I have a radon problem?
A. No. Radon levels vary from house to house. The only way to know if you have a radon problem is to conduct a test.
- State and Regional Radon Contacts
- Additional Information Sources
- Suggested Reading List
Council on Scientific Affairs. 1987. American Medical Association (AMA), Radon in Homes. Journal of the American Medical Association. 258:668-672.
Council on Scientific Affairs. 1991. Health Effects of Radon Exposure. Archives of Internal Medicine. 151:674-677.
Lubin, J.M., Samet and Weinberg, C. 1990. Design Issues in Epidemiologic studies of Indoor Exposure to Rn and Risk of Lung Cancer. Health Physics. 59(6): 807-817.
National Academy of Sciences, 1991. Comparative Dosimetry of Radon in Mines and Homes. National Academy Press, Washington, DC.
National Academy of Sciences, 1988. Health Risk of Radon and Other Internally Deposited Alpha Emitters; BEIR IV. National Academy press, Washington, DC.
Roscoe, R.J., et al. 1989. Lung Cancer Mortality Among Non-Smoking Uranium Miners Exposed to Radon Daughters. Journal of the American Medical Association. 262(5): 629-633.
Samet, J.M., Stolwijk, J. and Rose, S. 1991a. Summary: International Workshop on Residential Rn Epidemiology. Health Physics. 60(2):223-227.
Samet, J.M. and Hornung, R. 1990. Workshop on Indoor Air Quality: Review of radon and Lung Cancer Risk. Risk Analysis. 10(1): 65-75.
U.S. DOE/Office of Energy Research, 1989. International Workshop on Residential Radon Epidemiology: Workshop Proceedings. Commission of European Communities, Radiation Protection Program. CONF-8907178.
